Retinopathy of Prematurity
Neonatal Disease
Complete post test after you read this module. Save your certificate of completion!
Retinopathy of Prematurity
Overview:
Retinopathy of Prematurity (ROP) is a disorder of the eye that can affect premature infants, especially those born before 31 weeks of gestation or with a birth weight less than 1,250 grams. ROP is characterized by abnormal blood vessel development in the retina, the light-sensitive tissue at the back of the eye.
1. Pathophysiology:
The normal development of retinal blood vessels is incomplete in premature infants. In ROP, the
blood vessels may grow abnormally, leading to two main stages:
Normal Retinal Vascular Development
In utero development: Retinal vascularization begins around the 16th week of gestation and
completes near term (40 weeks).
The retina vascularizes from the optic nerve outward, with the temporal retina being the last
area to develop.
Premature Birth and Disrupted Retinal Vascularization
Premature birth interrupts normal vascularization, leaving parts of the retina avascular.
Retinal vessels are exposed to extrauterine conditions, which can disrupt their development.
Hypoxia-Induced Vascular Regression
After premature birth, the retina remains metabolically active but lacks adequate vascular supply.
The avascular retina becomes relatively hypoxic, leading to:
Release of vasoactive and angiostatic factors like VEGF (vascular endothelial growth factor) and IGF-1 (insulin-like growth factor 1).
Initial suppression of VEGF due to hyperoxia from supplemental oxygen therapy or immature oxygen regulation.
Phase I: Hyperoxia and Vascular Stasis (Birth to 30-32 Weeks)
Excessive oxygenation from supplemental oxygen leads to hyperoxia, downregulating VEGF and causing:
Arrested vascular growth.
Retinal vessel obliteration.
Peripheral avascular retina persists.
Phase II: Hypoxia and Pathological Neovascularization (32-34 Weeks and Beyond)
As the infant matures and oxygen supplementation decreases, the avascular retina becomes hypoxic.
Hypoxia triggers a surge in VEGF and other proangiogenic factors, leading to:
Abnormal neovascularization: Fragile, disorganized vessels grow into the vitreous instead of the retina.
These vessels are prone to leakage and hemorrhage.
Retinal Detachment and Vision Loss
Untreated ROP progresses to:
Fibrovascular proliferation: Scarring and contraction of abnormal vessels.
Tractional retinal detachment: Leading to permanent vision impairment or blindness.
2. Risk Factors:
Prematurity: The main risk factor is being born before 31 weeks of gestation.
Low Birth Weight: Infants with a birth weight less than 1,250 grams are at higher risk.
Oxygen Therapy: High levels of oxygen therapy, especially in the first weeks of life, contribute to the development of ROP.
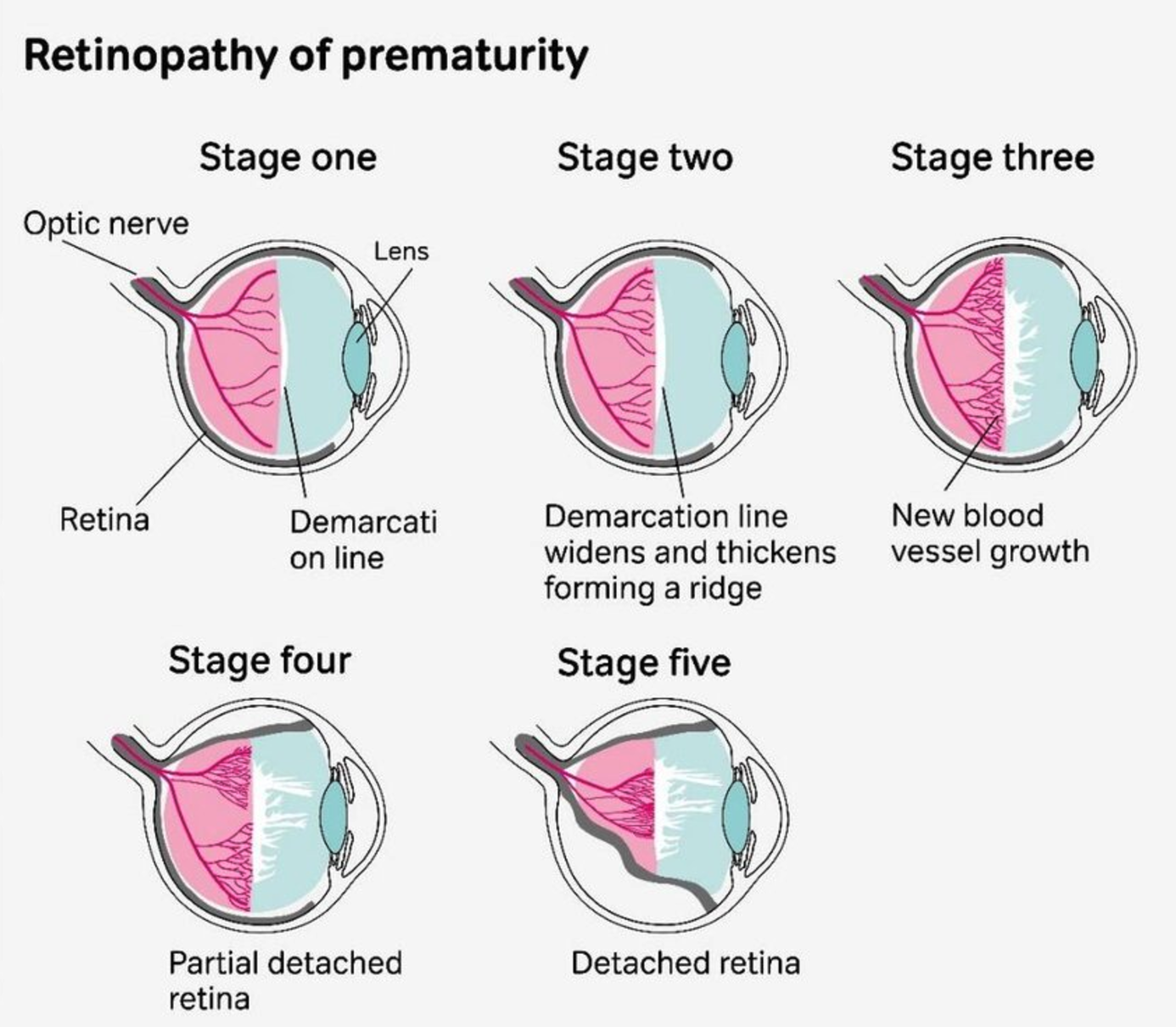
3. Clinical Staging:
Stage 1: Demarcation line between vascular and avascular retina.
Stage 2: Ridge formation with elevated tissue.
Stage 3: Extraretinal neovascularization.
Stage 4: Partial retinal detachment.
Stage 5: Total retinal detachment.
4. Management:
Monitoring:
Regular eye examinations to detect and monitor ROP are crucial.
Exams are typically done using a special instrument to visualize the retina.
Treatment:
Treatment may be needed if the disease progresses to a severe stage.
Laser therapy or cryotherapy is used to stop the abnormal blood vessel growth.
5. Preventing Retinopathy of Prematurity (ROP): Specific Strategies for NICU RTs
Neonatal Intensive Care Unit (NICU) Respiratory Therapists (RTs) play a crucial role in preventing Retinopathy of Prematurity (ROP) by implementing specific strategies aimed at minimizing risk factors associated with this eye disorder. Here are key measures:
Oxygen Management:
Specifics: NICU RTs must closely monitor and control oxygen levels, avoiding both hypoxia and hyperoxia. Studies show SPO2 levels may be safer at 90-95% for low-birth-weight babies.
Explanation: Maintaining oxygen within target ranges, often guided by pulse oximetry, helps prevent fluctuations that contribute to ROP. The goal is to strike a balance between adequate oxygenation and avoiding excessive oxygen exposure. Find out what your hospital's protocols are for oxygen saturations.
Oxygen Saturation Targets:
Explanation: Oxygen saturation targets are carefully determined based on the infant's gestational age and clinical condition. RTs must ensure that oxygen levels remain within these defined ranges to mitigate the risk of ROP development.
Use of Pulse Oximetry:
Explanation: Continuous monitoring enables prompt detection of oxygen saturation variations, allowing for timely adjustments in oxygen therapy. RTs play a crucial role in interpreting and responding to pulse oximetry readings.
Collaboration with Ophthalmologists:
Explanation: RTs work in tandem with ophthalmologists to ensure that infants at risk of ROP receive timely and appropriate eye examinations. Early detection allows for intervention when necessary.
Implementation of Low Oxygen Levels:
Explanation: Keeping oxygen levels toward the lower end of the target range helps minimize exposure, reducing the risk of oxygen-induced vascular changes in the retina.
Avoidance of Sudden Oxygen Changes:
Explanation: Abrupt changes in oxygen concentration can contribute to the development of ROP. RTs should implement gradual adjustments to prevent fluctuations that may adversely
Review of Respiratory Care Protocols:
Explanation: Staying informed about the latest evidence-based practices in respiratory care allows RTs to implement protocols that align with current standards, optimizing respiratory support while minimizing the risk of ROP.
6. NICU RT's Role and Actions:
Assessment:
The NICU Respiratory Therapist (RT) begins by assessing the baby's current respiratory status, including respiratory rate, breath sounds, and the effectiveness of the current NIPPV support.
Communication with Ophthalmology:
Collaborates with the ophthalmology team to understand the severity of ROP and the need for ongoing eye exams. Maintains open communication to stay informed about any changes in the baby's retinal status.
Monitoring:
Monitors the baby's vital signs, including heart rate and respiratory rate, continuously. Regularly assesses the baby's response to respiratory interventions, especially high doses of 02 for prolonged periods of time.
Maintaining Oxygen Targets:
Implements strategies to keep oxygen saturation within the recommended target range, aiming to minimize the risk of ROP progression while avoiding the adverse effects of hyperoxia. Always refer to your hospital policies for target SPO2 ranges.
Fun Fact!
First Identification in 1942
ROP was first described in 1942 by Dr. Theodore Terry, who initially called it “retrolental fibroplasia” (RLF). This term highlighted the condition's hallmark: fibrous tissue growing behind the lens due to retinal detachment.