Prostaglandin
Medication
Complete post test after you read this module. Save your certificate of completion!
Prostaglandin
Overview:
Prostaglandins are a group of lipid compounds that are derived from fatty acids and play a crucial role in various physiological processes in the body. They were first discovered in the prostate gland, which is how they got their name. Prostaglandins are short-lived and act locally, exerting their effects near the site of synthesis.
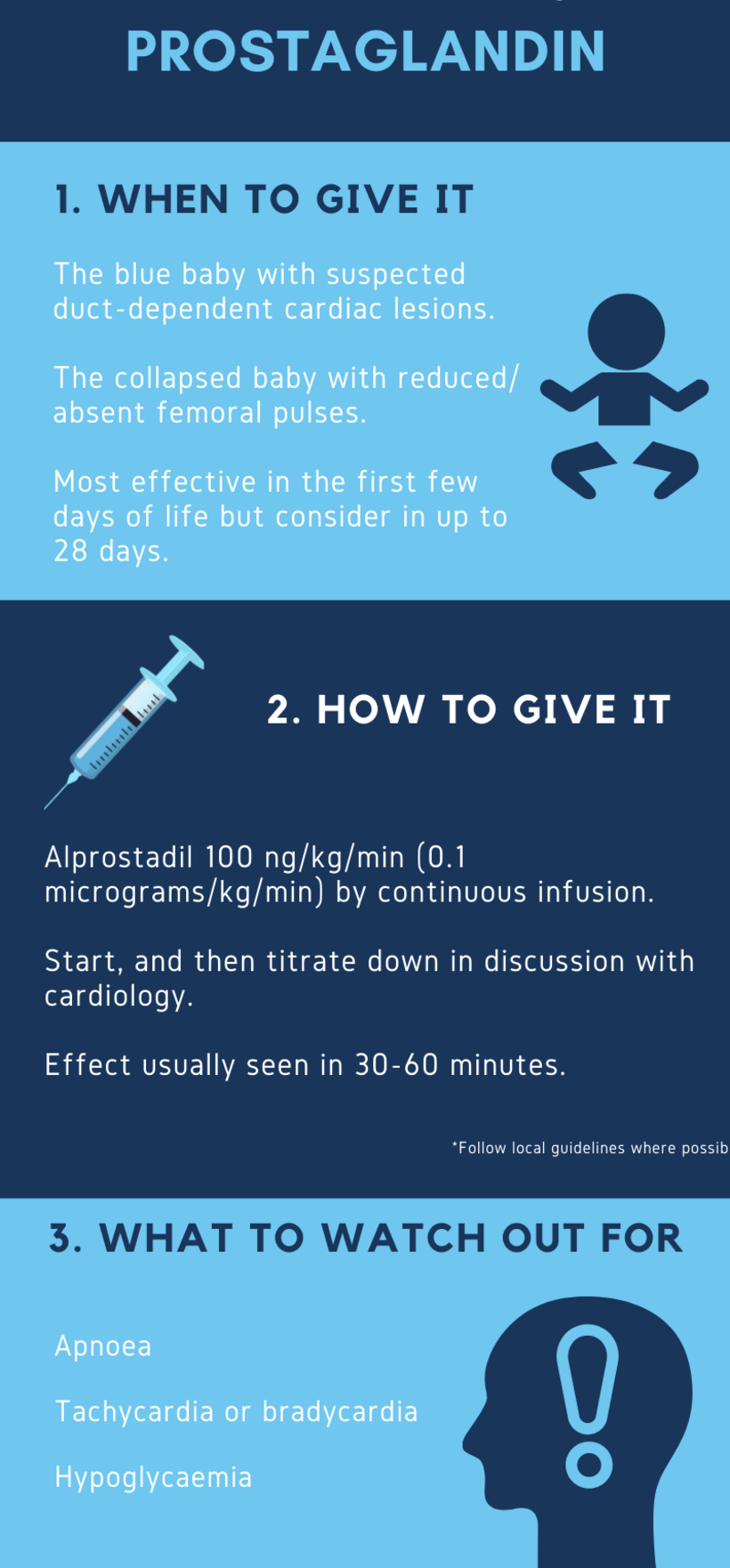
1. Indications in Neonates:
Patent Ductus Arteriosus (PDA) Closure: Prostaglandin E1 (PGE1), commonly known as alprostadil, may be administered in neonates to keep the ductus arteriosus open in specific cardiac conditions, allowing for adequate oxygenation until corrective measures can be taken.
Neonatal Tetralogy of Fallot: In some cases, prostaglandins can be used to maintain ductal patency in neonates with Tetralogy of Fallot, a congenital heart defect.
Pulmonary Hypertension: Prostaglandins may be considered in neonates with persistent pulmonary hypertension of the newborn (PPHN) to help maintain ductal patency and improve pulmonary blood flow.
2. Contraindications in Neonates:
Structurally Normal Hearts: Prostaglandins should not be used in neonates with structurally normal hearts, as maintaining
ductal patency is unnecessary and could lead to complications.
Congenital Heart Defects Requiring Ductal Closure: In cases where a neonate has a congenital heart defect that
necessitates ductal closure, the use of prostaglandins may be contraindicated.
Hypersensitivity: Neonates with known hypersensitivity or allergic reactions to prostaglandins, specifically alprostadil,
should not receive these medications.
3. Special Circumstances in Neonates:
Monitoring: Continuous monitoring of neonates receiving prostaglandins is essential. This includes monitoring vital signs, oxygen
saturation, and response to therapy.
Dosage Adjustments: Prostaglandin therapy may require individualized dosage adjustments based on the neonate's response and
specific clinical condition.
Duration of Treatment: The duration of prostaglandin treatment is determined by the underlying condition. For example, in PDA closure, the goal is often to maintain ductal patency until corrective measures, such as surgery, can be performed.
Potential Side Effects: Prostaglandin therapy may be associated with side effects such as apnea, fever, and diarrhea. Neonates should be carefully monitored for these effects.
Transition to Definitive Treatment: Prostaglandin therapy is often a bridge to definitive treatment, especially in cardiac conditions. Planning for and executing the transition to surgical or other interventions is a critical aspect of neonatal care.
4. Key Functions:
Inflammation Regulation: Prostaglandins are known for their role in inflammation. They mediate the inflammatory response, causing vasodilation and increasing vascular permeability. This contributes to the characteristic signs of inflammation, such as redness, heat, swelling, and pain.
Smooth Muscle Contraction and Relaxation: Prostaglandins have a significant impact on smooth muscle activity. They can either promote or inhibit smooth muscle contraction, depending on the specific receptors they bind to.
Platelet Aggregation and Blood Clotting: Some prostaglandins influence platelet function and blood clotting. They can either enhance or inhibit platelet aggregation, playing a role in hemostasis and blood clot formation.
Fever Induction: Prostaglandins, particularly PGE2, are involved in the regulation of body temperature. They act on the hypothalamus, contributing to the induction of fever during an immune response.
Reproductive Processes: Prostaglandins play a crucial role in various aspects of reproductive physiology. They are involved in uterine contractions during labor and menstruation, as well as in the regulation of blood flow to the reproductive organs.
5. Use on Neonates
a. Maintaining a Patent Ductus Arteriosus (PDA)
In certain congenital heart defects, such as hypoplastic left heart syndrome, transposition of the great arteries, or pulmonary atresia, the heart's blood flow is critically dependent on the patency of the ductus arteriosus. Normally, this fetal blood vessel closes shortly after birth, but in these cases, it must remain open for the infant to survive. PGE1 is administered to keep the ductus arteriosus open, allowing for better oxygenation and systemic blood flow. If prostaglandin therapy is not administered or fails, the infant may experience severe hypoxia and cardiovascular collapse. As RTs manage the infant's respiratory needs, understanding the connection between ventilation and oxygenation and how PGE1 affects circulation helps in early recognition of complications and proper ventilation support.
b. Assessment of Oxygenation and Ventilation Needs
When an infant receives prostaglandin therapy, the RT needs to carefully monitor the infant’s oxygenation and ventilation status. The opened ductus can affect the balance of blood flow between the lungs and the rest of the body, and this can lead to abnormal ventilation-perfusion (V/Q) matching. RTs will need to assess the infant's oxygen saturation and adjust ventilator settings to ensure effective gas exchange. The interplay between prostaglandin use and respiratory support means RTs need to be aware of the potential for hypoxemia or respiratory distress, and they must be prepared to adjust oxygen therapy or mechanical ventilation as needed.
c. Implications for Respiratory Management
Infants on prostaglandin therapy may require higher levels of respiratory support because the ductus arteriosus, though kept open, may alter the normal hemodynamics of the circulatory and respiratory systems. RTs may be asked to help manage respiratory complications like pulmonary edema, tachypnea, or increased work of breathing, all of which may occur as a result of altered blood flow. Prostaglandin use can also lead to hypotension, which may further complicate ventilation. RTs should be prepared to adjust interventions, including CPAP, non-invasive ventilation, or mechanical ventilation, based on the infant's hemodynamic and respiratory status.
6. Clinical Significance:
Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) work by inhibiting the activity of cyclooxygenase, thereby reducing the synthesis of prostaglandins. This action provides relief from pain and inflammation.
Cardiovascular Medications: Prostaglandins play a role in regulating blood flow and blood pressure. Medications targeting prostaglandin pathways are used in certain cardiovascular conditions.
7. Complications:
Apnea: Babies may temporarily stop breathing. They may need extra breathing support like CPAP or ventilation.
Bradycardia: The heart rate may become too slow, which might require treatment like atropine to speed it up.
Low Blood Pressure (Hypotension): Prostaglandin can lower blood pressure, which may require fluids or medication to stabilize.
Fever: Some babies get a mild fever as a side effect, which should be monitored.
Flushing: The skin may turn red or warm due to changes in blood flow. This is usually not serious but should be watched.
Gastrointestinal Issues: Rarely, babies might experience diarrhea or vomiting, which could lead to dehydration.
Brain Bleeding: In very sick or premature babies, low blood pressure from prostaglandin could increase the risk of brain bleeding.
Why is important for an RT to understand Prostaglandin?
Keeps the Ductus Arteriosus Open: In some heart defects, the baby’s blood flow depends on keeping a blood vessel (the ductus arteriosus) open. Prostaglandin (PGE1) is used to keep this vessel open, allowing the baby to survive. RTs need to understand this so they can manage the baby’s oxygen levels and breathing properly.
Affects Oxygenation and Ventilation: Prostaglandin can change blood flow, which might affect how well the baby’s lungs get oxygen. RTs need to monitor oxygen levels carefully and adjust ventilator settings if needed.
More Respiratory Support Needed: Babies on prostaglandin therapy may need more help with breathing, like extra oxygen or ventilator support, due to changes in blood flow. RTs need to be prepared to adjust care as the baby’s condition changes.
Watch for Side Effects: Prostaglandin can cause side effects like bradycardia (slow heart rate), low blood pressure, and apnea (temporary stopping of breathing). RTs should be alert to these issues and ready to intervene if needed.